Table of Contents
Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition that affects millions of people worldwide. It can lead to a reduced quality of life, limited physical activity, and impaired lung function. While COPD cannot be cured, various therapeutic Exercises for COPD patients can help manage its symptoms and improve overall well-being. This article explores a range of therapeutic exercises for COPD patient, including stretching exercises, resistance training, manual stretching, joint mobilization, soft tissue manipulation, balance exercises, core strengthening, postural correction, TENS therapy, ultrasound therapy, heat therapy, cold therapy, electrical stimulation, hydrotherapy, cupping therapy, myofascial release, trigger point therapy, proprioceptive exercises, neuromuscular reeducation, Pilates, Yoga therapy, McKenzie method, Mulligan concept, Maitland technique, and nerve gliding exercises, that can benefit COPD patients in their journey towards better health.
1. Understanding COPD
1.1. What is COPD?
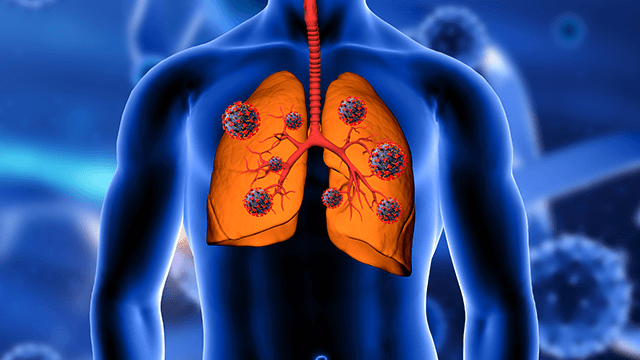
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by obstructed airflow and breathing difficulties. It includes conditions such as chronic bronchitis and emphysema. COPD is mainly caused by smoking and long-term exposure to air pollutants.
1.2. Causes and Risk Factors
Cigarette smoking is the primary cause of COPD, accounting for about 90% of cases. Other risk factors include exposure to secondhand smoke, air pollution, occupational dust and chemicals, genetic factors (alpha-1 antitrypsin deficiency), and respiratory infections.
1.3. Symptoms and Diagnosis
Common symptoms of COPD include chronic cough, excessive sputum production, shortness of breath (dyspnea), wheezing, and chest tightness. A medical history assessment and lung function tests, such as spirometry and lung volume measurements, are used to diagnose COPD.
1.4. Importance of Exercise
Regular exercise is vital for COPD patients. It helps strengthen respiratory muscles, improve lung function, enhance overall physical conditioning, reduce symptoms, and improve quality of life.
2. Therapeutic Exercises for COPD Patient
Here are the top 15 most therapeutic exercises for COPD patient:
2.1. Stretching for COPD Patients
Stretching exercises can be beneficial for individuals with Chronic Obstructive Pulmonary Disease (COPD) as they can help improve flexibility, lung function, and overall physical well-being. However, before starting any exercise routine, it’s crucial for COPD patients to consult with their healthcare provider or a pulmonary rehabilitation specialist to ensure they’re performing exercises suitable for their specific condition.

TYPES OF STRETCHING EXERCISES
Here are some general stretching therapeutic exercises for COPD patients:
- Neck Stretch: Gently tilt your head to one side, bringing your ear toward your shoulder. Hold for 15-30 seconds and repeat on the other side.
- Shoulder Stretch: Clasp your hands behind your back and straighten your arms while lifting your chest. Hold for 15-30 seconds.
- Chest Stretch: Stand with your arms at shoulder height against a wall or door frame, then lean forward slightly until you feel a stretch in your chest muscles. Hold for 15-30 seconds.
- Arm Reach: Raise one arm overhead and reach upwards, feeling the stretch along your side. Hold for 15-30 seconds and repeat on the other side.
- Trunk Rotation: Sit or stand with your feet shoulder-width apart, then gently twist your upper body to the left and right, keeping your hips stable. Hold each side for 15-30 seconds.
- Quadriceps Stretch: Stand near a wall or a sturdy chair for balance. Bend one knee and bring your heel toward your buttocks, holding the ankle with your hand. Hold for 15-30 seconds and switch to the other leg.
- Hamstring Stretch: Sit on the edge of a chair with one leg extended straight in front of you. Lean slightly forward from your hips until you feel a gentle stretch in the back of your thigh. Hold for 15-30 seconds and switch to the other leg.
- Calf Stretch: Stand facing a wall with your hands on it. Step one foot back and press the heel down to stretch the calf muscle. Hold for 15-30 seconds on each leg.
- Deep Breathing Exercises: Inhale slowly through your nose, expanding your abdomen, and then exhale slowly through pursed lips, as if you are blowing out a candle. This can help improve lung function and relaxation.
There are two common types of stretching: static stretching and dynamic stretching. Static stretching involves holding a stretch for a prolonged period, while dynamic stretching involves moving through a range of motion. Both types can be beneficial for COPD patients.
Precautions and Safety Tips
COPD patients should start stretching exercises slowly and avoid bouncing or jerking movements. It’s essential to maintain proper form during stretching to prevent injuries. Consult a healthcare professional before beginning any exercise program, especially if you have other medical conditions or concerns.
2.2. Resistance Training for COPD
Resistance training, also known as strength training or weight training, can be highly beneficial for individuals with Chronic Obstructive Pulmonary Disease (COPD). When done correctly and under the guidance of a healthcare professional or physiotherapist, resistance training can help improve muscle strength, endurance, and overall physical capacity, which can have positive effects on COPD symptoms and functional abilities. Before starting any resistance training program, it’s essential for COPD patients to consult with their healthcare provider or pulmonary rehabilitation specialist to ensure the exercises are safe and suitable for their specific condition.

Here are some key points to consider when incorporating resistance training therapeutic exercises for COPD patients:
- Start Slowly: If you’re new to resistance training or have not exercised in a while, begin with light weights or resistance bands and gradually increase the intensity as you become more comfortable and stronger. Over time, this will help prevent overexertion and reduce the risk of injury.
- Focus on Major Muscle Groups: Targeting major muscle groups, such as the legs, arms, chest, back, and core, will help improve overall body strength and functional capacity.
- Use Proper Breathing Techniques: Breathing is crucial for COPD patients during exercise. Practice controlled breathing techniques, such as pursed-lip breathing, to support your respiratory function during each exercise.
- Use Free Weights or Resistance Bands: Free weights (dumbbells) and resistance bands are excellent choices for resistance training. They allow for a wide range of motion and can be adjusted to suit your fitness level.
- Perform Compound Exercises: Compound exercises involve multiple joints and muscle groups working together. Examples include squats, lunges, chest presses, and rows. These exercises mimic real-life movements and are more functional for daily activities.
- Monitor Your Heart Rate: Keep an eye on your heart rate during exercise, and avoid pushing yourself too hard. Aim for a moderate level of exertion, where you can still talk comfortably while exercising.
- Rest and Recovery: Allow sufficient rest between exercise sessions to allow your muscles to recover and adapt.
- Work with a Qualified Trainer: If possible, work with a certified fitness trainer who has experience working with COPD patients. They can design a customized exercise plan and provide guidance on proper form and technique.
- Stay Hydrated: Drink plenty of water before, during, and after your workouts to stay hydrated.
- Listen to Your Body: If you experience any pain, dizziness, or significant shortness of breath during exercise, stop immediately and seek medical attention if necessary.
2.3. Manual Stretching and Joint Mobilization
Manual Stretching Techniques
Manual stretching and joint mobilization can be valuable components of a comprehensive rehabilitation program for COPD patients. These Therapeutic Exercises, when performed by trained physiotherapists, can help improve flexibility, joint mobility, and overall physical functioning in individuals with Chronic Obstructive Pulmonary Disease (COPD).

Manual Stretching: Manual stretching involves the application of gentle external force to lengthen and elongate muscles, tendons, and connective tissues. For COPD patients, manual stretching can be particularly beneficial in reducing muscle tightness, improving range of motion, and enhancing overall physical comfort. Common manual stretching therapeutic exercises for COPD patients include:
Hamstring Stretch: The therapist gently extends the leg while the patient is lying down or sitting, targeting the muscles in the back of the thigh.
Quadriceps Stretch: The therapist gently flexes the patient’s knee, bringing the heel toward the buttocks, targeting the muscles in the front of the thigh.
Chest Stretch: The therapist assists the patient in opening the chest and shoulders, which can help counteract the hunched posture often associated with COPD.
Joint Mobilization Exercises
Joint mobilization involves the skilled and controlled movement of joints by a therapist to improve joint function and reduce stiffness. It can be especially useful for COPD patients who may experience limitations in joint mobility due to inactivity or muscle tightness. Joint mobilization techniques should be gentle and within the patient’s pain-free range of motion. Examples of joint mobilization therapeutic exercises for COPD patients include:

Shoulder Mobilization: The therapist gently moves the patient’s shoulder joint in various directions to improve mobility and reduce stiffness.
Spinal Mobilization: The therapist applies gentle, rhythmic movements to the spine to enhance spinal mobility and reduce discomfort.
2.4. Soft Tissue Manipulation for COPD Relief
Understanding Soft Tissue Therapy
Soft tissue manipulation, also known as soft tissue mobilization or massage therapy, can provide relief and various benefits for individuals with Chronic Obstructive Pulmonary Disease (COPD). Soft tissue manipulation involves the manual manipulation of muscles, tendons, ligaments, and other soft tissues in the body. When performed by a trained and licensed Physical therapist, it can offer the following therapeutic exercises for COPD patients:

Techniques for COPD Patients
Muscle Relaxation: Soft tissue manipulation can help relax tense muscles and reduce muscle spasms, which may be beneficial for COPD patients who often experience muscle tightness and discomfort due to breathing difficulties and limited physical activity.
Improved Circulation: Massage therapy can promote better blood flow to the muscles and tissues, potentially enhancing oxygen and nutrient delivery to the affected areas. Improved circulation can also aid in the removal of waste products, reducing muscle soreness and fatigue.
Enhanced Breathing Mechanics: Certain massage techniques, particularly those targeting the chest, back, and ribcage, can help improve respiratory muscle function and breathing mechanics. This may lead to increased lung expansion and better airflow.
Stress Reduction: COPD can be associated with increased stress and anxiety. Soft tissue manipulation can promote relaxation, reduce stress hormones, and improve overall mental well-being, which may positively impact COPD symptoms.
Pain Management: Massage therapy can help alleviate localized pain and discomfort associated with COPD, providing a non-invasive and drug-free option for pain management.
Joint Mobility: By releasing tension in soft tissues surrounding joints, soft tissue manipulation can improve joint mobility and flexibility, which can be beneficial for COPD patients who may experience joint stiffness due to reduced physical activity.
Enhanced Sleep: Improved relaxation and reduced discomfort from soft tissue manipulation can lead to better sleep quality, which is important for overall health and well-being, especially for individuals with COPD.
2.5. Balance Exercises for Improved Stability
Balance Training and COPD
Balance exercises are essential for improving stability and reducing the risk of falls for individuals with Chronic Obstructive Pulmonary Disease (COPD). COPD can lead to reduced physical activity, muscle weakness, and decreased lung function, all of which can contribute to balance issues. Incorporating balance exercises into a comprehensive COPD management plan can help enhance stability and overall physical functioning. Before starting any exercise program, COPD patients should consult with their healthcare provider or pulmonary rehabilitation specialist to ensure the exercises are safe and appropriate for their condition.

Balance Therapeutic Exercises for COPD Patients TO REDUCE FALL RISKS
Single Leg Stance: Stand near a stable surface, such as a countertop or chair, and lift one leg off the ground, bending your knee at a 90-degree angle. Try to maintain your balance for 10-30 seconds, then switch to the other leg. If needed, lightly touch the stable surface for support.
Heel-to-Toe Walk: Walk in a straight line, placing the heel of one foot directly in front of the toes of the other foot with each step. This exercise helps improve balance and coordination.
Tandem Stance: Stand with one foot directly in front of the other, so the heel of the front foot touches the toes of the back foot. Hold this position for 10-30 seconds, then switch foot positions. Use a stable surface for support if necessary.
Standing Leg Swings: Stand near a stable surface and swing one leg forward and backward, like a pendulum. Repeat 10-15 swings on each leg. This exercise challenges balance and strengthens hip muscles.
Side Leg Raises: Stand near a stable surface and lift one leg out to the side while keeping your upper body stable. Repeat 10-15 raises on each leg. This exercise targets the hip abductor muscles.
Chair Sit-Stand: Sit in a chair and practice standing up without using your hands. Then, slowly lower yourself back into the chair. Repeat this movement 10-15 times to strengthen leg muscles and improve balance during transitions.
Rock the Boat: Stand with your feet shoulder-width apart and gently shift your weight from side to side, keeping your movements controlled. This exercise challenges balance and activates core muscles.
Modified Yoga Poses: Gentle yoga poses, such as Tree Pose (Vrksasana) or Warrior II (Virabhadrasana II), can help improve balance, flexibility, and strength for COPD patients. Always perform these poses with the support of a chair or wall for stability.
Ankle Circles: Sit in a chair with your feet flat on the ground. Lift one foot and rotate your ankle in a circular motion clockwise and then counterclockwise. Repeat 5-10 circles in each direction and then switch to the other foot.
2.6. Core Strengthening for Better Respiratory Support
Importance of Core Muscles in COPD
Core strengthening therapeutic exercises for COPD patients can play a crucial role in providing better respiratory support for individuals with Chronic Obstructive Pulmonary Disease (COPD). A strong core helps support the diaphragm and other respiratory muscles, improving lung function, and making breathing more efficient. Strengthening the core can also enhance overall stability, balance, and posture, which can be beneficial for COPD patients who may experience muscle weakness and postural changes due to their condition.
Before starting any core strengthening exercises, it’s essential for COPD patients to consult with their healthcare provider or pulmonary rehabilitation specialist to ensure the exercises are safe and appropriate for their specific condition and fitness level.

Core Strengthening Therapeutic Exercises for COPD Patients
Diaphragmatic Breathing: Diaphragmatic breathing, also known as belly breathing, is a fundamental exercise that helps strengthen the diaphragm and improve lung function. Sit or lie down comfortably and place one hand on your chest and the other on your abdomen. Inhale deeply through your nose, expanding your abdomen (the hand on your abdomen should rise), and then exhale slowly through pursed lips. Repeat this exercise several times a day to reinforce proper breathing mechanics.
Pelvic Tilt: Lie on your back with your knees bent and feet flat on the floor. Tighten your abdominal muscles and press your lower back into the floor while tilting your pelvis upward. Hold for a few seconds and then release. Repeat 10-15 times.
Bridges: Lie on your back with your knees bent and feet flat on the floor. Lift your hips off the ground until your body forms a straight line from shoulders to knees. Engage your core and glute muscles during the movement. Hold for a few seconds and then lower your hips back down. Repeat 10-15 times.
Dead Bug: Lie on your back with your arms extended toward the ceiling and your knees bent at a 90-degree angle. Slowly lower one arm and the opposite leg toward the floor, keeping your core engaged and back flat on the ground. Return to the starting position and repeat on the other side. Continue alternating sides for 10-15 repetitions.
Plank: Start in a push-up position with your hands directly under your shoulders and toes on the floor. Keep your body in a straight line from head to heels, engaging your core muscles throughout the exercise. Hold this position for as long as you can maintain proper form, gradually increasing the duration over time.
Seated Torso Twists: Sit on a chair with your feet flat on the floor and your hands clasped together in front of your chest. Slowly twist your torso to the right, then back to the center, and then to the left. Repeat 10-15 twists on each side.
Standing Side Bends: Stand with your feet shoulder-width apart and your hands on your hips. Gently bend to one side, sliding your hand down the side of your leg while keeping your core engaged and shoulders level. Return to the center and then repeat on the other side. Do 10-15 repetitions on each side.
2.7. Postural Correction to Enhance Breathing
Postural correction is essential for individuals with Chronic Obstructive Pulmonary Disease (COPD) to enhance breathing efficiency and optimize lung function. COPD can lead to changes in posture, such as a forward-leaning or hunched position, which can restrict lung expansion and make breathing more challenging. Improving posture through simple adjustments can help open up the chest, improve respiratory muscle function, and support better breathing.

Postural Correction Tips
Here are some postural correction therapeutic exercises for COPD patients to enhance breathing
Sit and Stand Tall: When sitting or standing, aim to maintain an upright posture with your shoulders back and relaxed. Avoid slouching or hunching forward, as this can compress the chest and reduce lung capacity. Imagine a string pulling you gently upward from the top of your head.
Engage Your Core: Gently engage your abdominal muscles to support your spine and maintain an aligned posture. This can also aid in diaphragmatic breathing, allowing the diaphragm to move more freely for efficient breathing.
Adjust Your Chair: If you spend extended periods sitting, choose a chair that provides proper lumbar support and keeps your feet flat on the floor. Avoid chairs that cause you to slouch or lean forward excessively.
Elevate Your Head During Sleep: If possible, elevate the head of your bed or use an adjustable bed to sleep with your upper body slightly elevated. This can help reduce shortness of breath and alleviate nighttime breathing difficulties.
Chest Opening Exercises: Perform exercises that focus on opening up the chest and shoulders. Stretching the chest muscles and shoulder blades can improve chest expansion and allow for deeper breathing. Examples include chest stretches against a wall and shoulder rolls.
Avoid Crossing Legs: When sitting, avoid crossing your legs, as it can restrict blood flow and affect overall posture. Keep both feet flat on the floor and distribute your weight evenly.
Use Supportive Pillows: Use supportive pillows behind your back when sitting or resting to maintain proper spinal alignment and support a more upright posture.
Avoid Overreaching: When reaching for objects or performing activities, be mindful of your posture. Avoid overreaching or twisting excessively, as it can strain the chest and abdomen.
Stay Active: Engage in regular physical activity and exercises, including those that promote posture and balance. Strengthening the core and back muscles can also contribute to better posture.
Pursed-Lip Breathing: Practice pursed-lip breathing during daily activities, especially when you feel short of breath. This technique can help improve breathing efficiency and control.
2.8. Modalities for COPD Management
COPD management involves a comprehensive approach that may include various modalities to control symptoms, improve lung function, enhance quality of life, and reduce the frequency of exacerbations. The specific modalities used can vary depending on the severity of COPD and individual patient needs. Here are some common modalities used for COPD management:
Medications: Medications are a cornerstone of COPD management. Bronchodilators, such as short-acting and long-acting beta-agonists and anticholinergics, help relax the airway muscles and improve airflow. Inhaled corticosteroids may be prescribed for those with frequent exacerbations or significant inflammation. Other medications, such as phosphodiesterase-4 inhibitors, can help reduce inflammation and improve lung function.
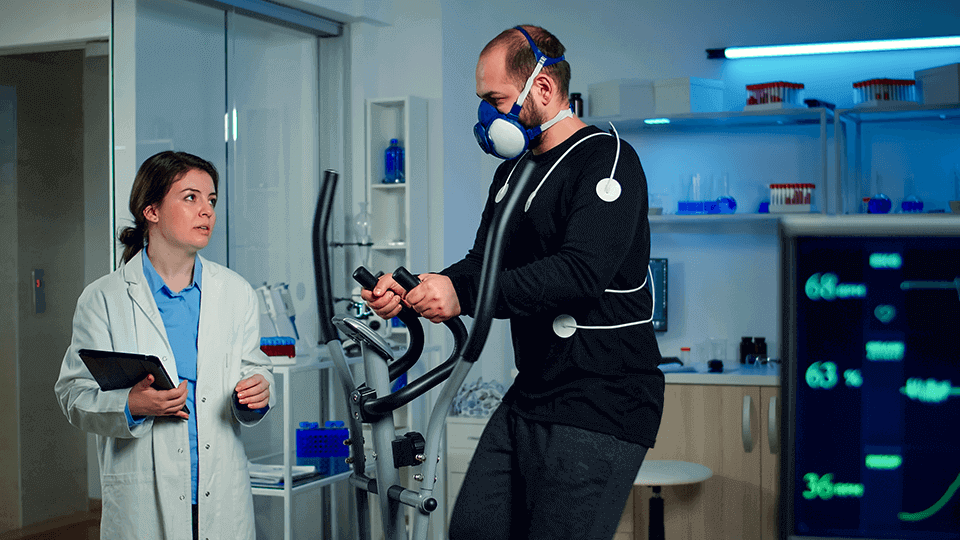
Pulmonary Rehabilitation: Pulmonary rehabilitation is a comprehensive program that includes exercise training, education, and support for COPD patients. It aims to improve exercise tolerance, breathing techniques, and overall physical functioning. Pulmonary rehabilitation can lead to reduced symptoms, increased quality of life, and better self-management of COPD.
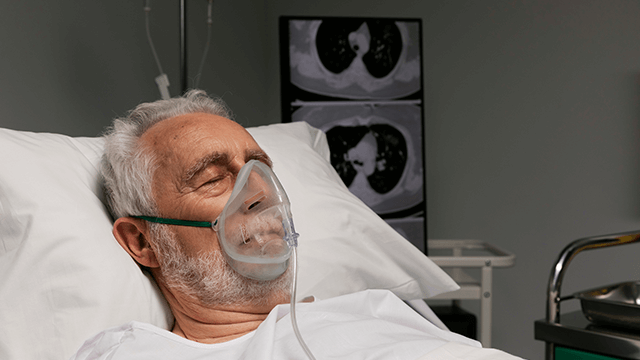
Oxygen Therapy: For individuals with severe COPD and low oxygen levels, supplemental oxygen therapy may be prescribed. Oxygen therapy can improve blood oxygen levels, reduce shortness of breath, and enhance exercise capacity.
Smoking Cessation Programs: Smoking is the leading cause of COPD, and quitting smoking is essential for slowing disease progression. Smoking cessation programs, counseling, and nicotine replacement therapies can assist patients in quitting smoking.
Breathing Exercises: Breathing exercises, such as diaphragmatic breathing and pursed-lip breathing, can help COPD patients control breathlessness and improve the efficiency of breathing.
Vaccinations: Annual flu vaccinations and pneumococcal vaccinations are recommended for COPD patients to reduce the risk of respiratory infections and exacerbations.
Nutritional Support: A balanced and healthy diet is important for COPD patients to maintain strength and overall health. Malnutrition can worsen COPD symptoms, so dietary guidance and nutritional support may be beneficial.
Home Oxygen Therapy: In cases of severe COPD, long-term home oxygen therapy may be prescribed to improve oxygen levels during rest and sleep.
Lung Volume Reduction Surgery: For select cases of severe emphysema, lung volume reduction surgery or bronchoscopy procedures may be considered to improve lung function and symptoms.
Lung Transplantation: For individuals with end-stage COPD and significant lung damage, lung transplantation may be an option.
2.9. Hydrotherapy and Its Benefits
Hydrotherapy, also known as aquatic therapy or water-based exercise, can be a beneficial and gentle form of physical therapy for COPD patients. Hydrotherapy involves performing exercises and movements in a pool or other water-based environment. The buoyancy of the water reduces the impact on the joints, making it a suitable option for individuals with COPD who may have limitations in their mobility or experience discomfort during weight-bearing exercises.

Here are some potential benefits of hydrotherapy therapeutic exercises for COPD patients:
Improved Breathing Efficiency: The warm water and the gentle resistance it provides can help enhance breathing mechanics and respiratory muscle function.
Muscle Relaxation: The warm water can promote muscle relaxation, reduce muscle tension, and alleviate discomfort.
Reduced Joint Stress: Hydrotherapy reduces the impact on the joints, making it easier and more comfortable for individuals with COPD to exercise and move.
Increased Flexibility and Range of Motion: Performing exercises in water can improve joint flexibility and range of motion, benefiting COPD patients who may have reduced mobility.
Enhanced Cardiovascular Endurance: Hydrotherapy exercises can be adapted to provide cardiovascular benefits without putting excessive strain on the respiratory system.
Improved Balance and Stability: Hydrotherapy exercises in a controlled environment can help improve balance and stability, reducing the risk of falls.
Enhanced Mood and Relaxation: The soothing and calming nature of water can promote relaxation and reduce stress, which can be beneficial for overall well-being.
2.10. Myofascial Release for Muscle Tension Reduction
Myofascial release is a manual therapy technique that targets the fascia, which is the connective tissue that surrounds and supports muscles, bones, and organs in the body. The goal of myofascial release is to release tension, adhesions, and restrictions in the fascia, promoting improved mobility, flexibility, and reduced pain.
While myofascial release is commonly used for various musculoskeletal conditions, its direct application for managing COPD itself is limited. COPD is a chronic respiratory condition primarily characterized by airflow limitation and lung tissue damage. The management of COPD primarily involves medical treatments, pulmonary rehabilitation, and lifestyle interventions aimed at improving respiratory function and overall well-being.

Therapeutic exercises for COPD patients:
Muscle Relaxation: Myofascial release can help relax tense muscles, reducing muscle tightness and discomfort that may be associated with COPD.
Improved Mobility: By releasing restrictions in the fascia, myofascial release may enhance joint mobility and overall flexibility.
Pain Relief: For COPD patients experiencing musculoskeletal pain, myofascial release can help alleviate pain and discomfort.
Postural Improvement: Myofascial release techniques may assist in correcting postural imbalances caused by altered breathing patterns.
2.11. Proprioceptive Exercises for Balance and Coordination
Proprioceptive exercises are beneficial for improving balance, coordination, and body awareness for individuals with COPD. These therapeutic exercises for COPD patients focus on enhancing the body’s ability to sense its position and movement in space, which can help prevent falls and improve overall physical functioning. COPD patients may experience reduced physical activity and muscle weakness, which can impact balance and coordination. Incorporating proprioceptive exercises into their routine can aid in addressing these issues. Before starting any exercise program, COPD patients should consult with their healthcare provider or pulmonary rehabilitation specialist to ensure the exercises are safe and suitable for their condition.

Here are some proprioceptive therapeutic exercises for COPD patients for balance and coordination:
Single Leg Balance: Stand near a stable surface, such as a countertop or chair, and lift one leg off the ground. Try to maintain your balance for as long as possible, aiming for 10-30 seconds. Then, switch to the other leg. Use the stable surface for support if needed.
Heel-to-Toe Walk: Walk in a straight line, placing the heel of one foot directly in front of the toes of the other foot with each step. This exercise challenges balance and coordination.
Tandem Stance: Stand with one foot directly in front of the other, so the heel of the front foot touches the toes of the back foot. Hold this position for 10-30 seconds, then switch foot positions. Use a stable surface for support if necessary.
Standing Leg Swings: Stand near a stable surface and swing one leg forward and backward like a pendulum. Repeat 10-15 swings on each leg. This exercise challenges balance and strengthens hip muscles.
Side Leg Raises: Stand near a stable surface and lift one leg out to the side while keeping your upper body stable. Repeat 10-15 raises on each leg. This exercise targets the hip abductor muscles.
Squat with Balance: Perform a squat while holding onto a stable surface for support. Then, rise up and balance on one leg for a few seconds before switching to the other leg.
Modified Yoga Poses: Gentle yoga poses, such as Tree Pose (Vrksasana) or Warrior II (Virabhadrasana II), can help improve balance, flexibility, and strength for COPD patients. Perform these poses with the support of a chair or wall for stability.
Rock the Boat: Stand with your feet shoulder-width apart and gently shift your weight from side to side, keeping your movements controlled. This exercise challenges balance and activates core muscles.
Ankle Circles: Sit in a chair with your feet flat on the ground. Lift one foot and rotate your ankle in a circular motion clockwise and then counterclockwise. Repeat 5-10 circles in each direction and then switch to the other foot.
2.12. Neuromuscular Reeducation for COPD Rehabilitation
Neuromuscular reeducation is a therapeutic approach used in COPD rehabilitation to help individuals with Chronic Obstructive Pulmonary Disease (COPD) regain control and coordination of their muscles, particularly those involved in breathing and other functional movements. COPD can lead to muscle weakness and altered movement patterns, which can affect breathing mechanics and overall physical function. Neuromuscular reeducation aims to retrain and optimize the neuromuscular pathways to improve muscle function and coordination.

In the context of COPD rehabilitation, neuromuscular reeducation can be beneficial for the following aspects:
Breathing Mechanics: COPD patients often experience breathing difficulties and may develop inefficient breathing patterns. Neuromuscular reeducation can help individuals learn proper diaphragmatic breathing techniques and enhance the coordination of respiratory muscles, leading to more efficient breathing.
Posture and Body Mechanics: COPD can lead to postural changes, muscle imbalances, and altered movement patterns. Neuromuscular reeducation can address these issues, promoting better posture and body mechanics during daily activities, which can help reduce strain on respiratory muscles.
Muscle Strength and Coordination: Neuromuscular reeducation exercises target specific muscle groups involved in breathing and functional movements. By focusing on muscle activation and coordination, COPD patients can improve muscle strength and enhance overall physical function.
Balance and Stability: COPD patients may experience balance issues, which can increase the risk of falls. Neuromuscular reeducation exercises can help improve balance and stability, reducing the risk of falls and related injuries.
Exercise Tolerance: Neuromuscular reeducation is often integrated into pulmonary rehabilitation programs, which include exercise training tailored to individual needs. By enhancing muscle function and coordination, COPD patients can improve exercise tolerance and physical endurance.
2.13. Mind-Body Practices: Pilates and Yoga Therapy
Mind-body practices, such as Pilates and yoga therapy, can be beneficial as complementary therapies for individuals with Chronic Obstructive Pulmonary Disease (COPD). These practices focus on the integration of physical movement, breathing techniques, and mindfulness to promote overall well-being, manage stress, and improve physical function. However, it is essential to consider the individual’s specific health condition and consult with a healthcare provider before starting any new exercise program, including Pilates and yoga therapy.

Pilates for COPD
Pilates is a low-impact exercise method that emphasizes core strength, flexibility, and proper alignment. It can be particularly beneficial for COPD patients as it promotes controlled breathing and improves posture, which can enhance breathing mechanics and reduce strain on respiratory muscles. Pilates exercises are adaptable to different fitness levels, and a qualified instructor can modify them to suit the individual’s needs and limitations.

Yoga Therapy for COPD
Yoga therapy involves the practice of physical postures (asanas), breathing exercises (pranayama), and relaxation techniques. For COPD patients, gentle yoga practices that focus on slow, controlled movements and deep breathing can help improve lung capacity, respiratory muscle strength, and overall physical well-being. Yoga also promotes relaxation and stress reduction, which can be beneficial for managing COPD-related anxiety and breathlessness.

Key benefits of Pilates and yoga therapeutic exercises for COPD patients include:
Improved Breathing: Both practices emphasize mindful breathing, which can help COPD patients enhance their breathing patterns and efficiency.
Core Strengthening: Pilates focuses on core strength, which supports better posture and can reduce strain on respiratory muscles.
Flexibility and Mobility: Both Pilates and yoga therapy can improve joint flexibility and overall mobility, making daily activities easier and reducing the risk of musculoskeletal issues.
Stress Reduction: Mindfulness and relaxation techniques in yoga and Pilates can reduce stress and anxiety, which can positively impact COPD management.
Enhanced Exercise Tolerance: Regular practice of Pilates and yoga can improve overall physical fitness and exercise tolerance, allowing COPD patients to engage in daily activities with greater ease.
Before starting Pilates or yoga therapy for COPD, it is essential to consider the following:
Consult with Healthcare Provider: Discuss your interest in Pilates or yoga therapy with your healthcare provider or pulmonary rehabilitation specialist to ensure it is safe and suitable for your individual condition.
Qualified Instructors: Work with qualified instructors who have experience in adapting exercises for individuals with COPD. They can tailor the practices to suit your specific needs and provide appropriate modifications.
Avoid Overexertion: Start with gentle and modified exercises, gradually increasing intensity as you build strength and confidence. Avoid overexertion or any movements that cause discomfort or breathlessness.
Listen to Your Body: Be mindful of how your body responds to the exercises. If you experience any pain or discomfort, stop the activity and rest.
2.14. Manual Therapy Techniques for COPD
McKenzie Method for COPD Relief
The McKenzie Method, also known as Mechanical Diagnosis and Therapy (MDT), is a specialized approach to evaluate and treat musculoskeletal conditions, particularly those involving the spine and extremities. While the McKenzie Method is not a primary treatment for COPD itself, it may be used as part of a comprehensive management plan to address musculoskeletal issues and improve functional movement in COPD patients.

Mulligan Concept for Improved Mobility
Assessment: A thorough evaluation is conducted to assess the patient’s movement patterns, posture, and specific musculoskeletal issues. The healthcare provider uses a standardized system to categorize and diagnose the problem.
Movement and Posture Correction: Based on the assessment, specific exercises and movements are prescribed to correct postural imbalances, improve joint mobility, and address movement dysfunctions.
Patient Empowerment: The McKenzie Method empowers patients to take an active role in managing their condition. Patients are taught self-treatment techniques and exercises they can perform independently to manage their musculoskeletal issues.
Directional Preference: The McKenzie Method emphasizes identifying the patient’s directional preference, meaning the specific movements that provide the most relief or improvement in symptoms. These movements are then incorporated into the treatment plan.
2.15. Nerve Gliding Exercises for COPD Nerve Pain
Nerve gliding therapeutic exercises for COPD patients, also known as neural gliding or neural mobilization exercises, are a set of specialized movements designed to improve the mobility and function of nerves. While nerve gliding exercises are not a primary treatment for COPD itself, they may be used as part of a comprehensive management plan to address nerve pain or discomfort that some COPD patients may experience due to various factors, such as altered breathing patterns, muscle imbalances, or reduced physical activity.

COPD patients may develop nerve pain or discomfort as a result of musculoskeletal issues, postural changes, or increased tension on nerves due to altered breathing mechanics. Nerve gliding exercises can help alleviate symptoms associated with nerve compression or irritation, improving overall comfort and function.
Here are some key points to consider regarding nerve gliding therapeutic exercises for COPD patients:
Specialized Movements: Nerve gliding therapeutic exercises for COPD patients involve specific movements that gently mobilize the nerves without causing undue tension or compression. These exercises are designed to glide and floss the nerves through their natural pathways.
Neural Tension Relief: Nerve gliding exercises can help release tension and reduce nerve compression, which may be contributing to pain or discomfort in COPD patients.
Individualized Approach: Nerve gliding exercises should be tailored to the individual’s specific symptoms and needs. A qualified healthcare professional or physical therapist with experience in neural mobilization can determine the appropriate exercises for the patient.
Caution and Gradual Progression: Nerve gliding exercises should be performed with caution and under the guidance of a healthcare professional to avoid exacerbating symptoms. The exercises should be introduced gradually, and any signs of increased pain or discomfort should be reported to the therapist.
Adjunct Therapy: Nerve gliding exercises should be used as part of a comprehensive COPD management plan that includes medical treatments, pulmonary rehabilitation, and other supportive therapies. They are not a standalone treatment for COPD or nerve pain.
3. Conclusion
Engaging in a tailored therapeutic exercise program that includes stretching, resistance training, manual therapy, and various modalities can significantly improve the quality of life for individuals living with COPD. It’s essential to work with healthcare professionals, such as physical therapists and fitness trainers, to create a safe and effective exercise plan. Regular practice of these exercises can lead to enhanced respiratory function, reduced pain, and improved overall well-being.
4. FAQs (Frequently Ask Questions)
Can stretching exercises cure COPD?
Stretching exercises cannot cure COPD, but they can improve lung function and alleviate breathing difficulties, leading to a better quality of life.
Is resistance training safe for individuals with COPD?
Yes, resistance training can be safe and beneficial for COPD patients when performed under appropriate guidance and supervision.
Add Your Heading Text Here
Are there any risks associated with manual stretching?
Manual stretching, when performed by a qualified professional, is generally safe. However, it’s essential to avoid overstretching to prevent injuries.
Can COPD patients perform balance exercises safely?
Yes, COPD patients can perform balance exercises, but it’s essential to start with simple exercises and progress gradually to prevent falls.
Are all the therapeutic techniques mentioned suitable for everyone with COPD?
No, the suitability of specific therapeutic techniques may vary from person to person. It’s best to consult with a healthcare professional to determine the most appropriate therapies for individual needs.