Table of Contents
Waking up with a stiff neck or developing a throbbing ache after hours at your desk can ruin your entire week. You turn your head to check your blind spot while driving, and a sharp, electric pain shoots down to your shoulder blade. You try to stretch it out, rub it, or crack it, but the tightness only seems to grab harder.
If you are currently experiencing this, you are not alone. Neck pain is the fourth leading cause of disability globally, with an estimated 30% of adults experiencing it annually. But here is the good news: while chronic issues often require a comprehensive treatment plan, acute flare-ups—that sudden “crick” in the neck or muscle spasm—can often be managed and significantly reduced within 48 hours if you follow the right protocol.
As a physical therapy expert, I have seen thousands of patients struggle with acute cervical pain. The mistake most people make is trying to force the neck to move before it is ready. This article outlines a clinically proven 3-Step Method designed to Reset, Release, and Re-engage your neck muscles.
This guide will not only help you reduce pain quickly but also help you distinguish between a simple muscle strain and a condition that requires an immediate neck pain physical therapist appointment.
The Anatomy of the Ache: What is Happening Inside Your Neck?
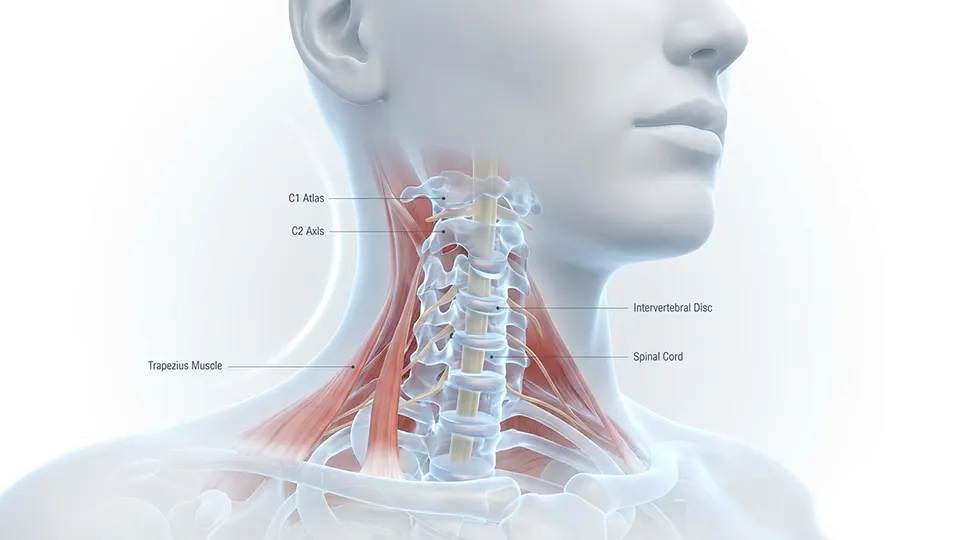
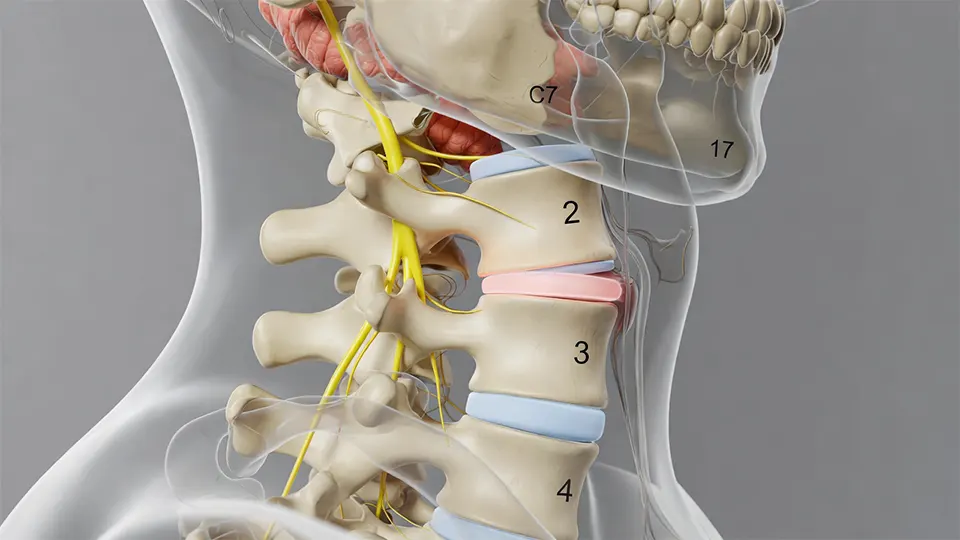
To fix the machine, you must understand the machine. Your neck, or cervical spine, is an engineering marvel. It consists of seven small vertebrae (C1-C7) stacked on top of one another, separated by shock-absorbing discs. This structure has a difficult job: it must balance your head—which weighs roughly 10 to 12 pounds (about the weight of a bowling ball)—while allowing a massive range of motion.
When you experience acute neck pain, it is usually due to one of three mechanical failures:
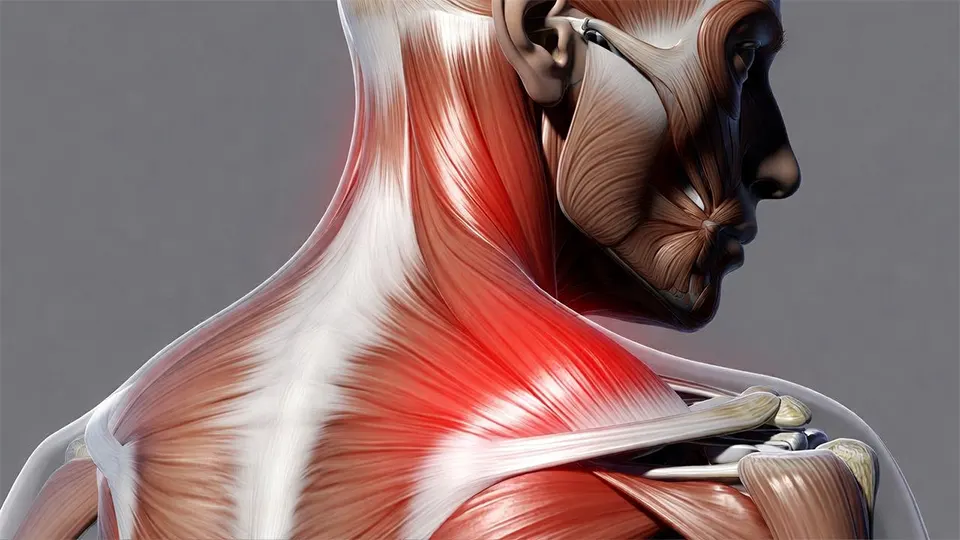
Muscular Guarding (The Spasm): This is your body’s defense mechanism. If you strain a small muscle or ligament, your brain sends a signal to the larger muscles (like the trapezius and levator scapulae) to “lockdown” the area. This splinting effect is what makes it impossible to turn your head.
Facet Joint Lock: The small joints that connect your vertebrae can sometimes get “stuck” or inflamed, often due to sleeping in an awkward position. This creates a sharp, pinpoint pain when you look in a specific direction.

Discogenic Irritation: The jelly-like discs between your vertebrae can bulge slightly, irritating the surrounding nerves. This often feels like a deep, dull ache that might radiate into the shoulder.
The 3-Step Method below primarily targets the first two categories—mechanical pain and muscular guarding—which account for the vast majority of acute neck pain cases.
Step 1: The "Reset" Phase (Hours 0–12)

Goal: Calm the neurological alarm system and reduce inflammation.
When your neck is in spasm, your muscles are in a state of panic. They are tightening up to protect the spine. Forcing them to stretch right now is like pulling on a knot—it will only get tighter. Step 1 is about convincing your nervous system that it is safe to relax.
1. The Zero-Gravity Decompression Pose

Gravity is currently your enemy. Every minute you spend upright requires your neck muscles to work. To “reset,” you need to take the weight of your head off your neck completely.
The Setup: Lie on your back on the floor (a yoga mat or carpet is fine). Do not use a pillow.
The Support: Take a small hand towel and roll it up into a cylinder about the thickness of your wrist. Place this roll under the curve of your neck, not under your head. Your head should rest flat on the floor, with the towel supporting the natural arch of your cervical spine.
The Action: Lie here for 10–15 minutes. Close your eyes and breathe deeply into your belly. This position places the spine in a neutral, unloaded state, signaling the paraspinal muscles to stop guarding.
2. Hydrotherapy: The Ice vs. Heat Debate

This is the most common question I get in the clinic. Here is the rule of thumb for the first 12 hours:
Ice (Cold Therapy): If the injury is fresh (under 24 hours), feels hot to the touch, or is throbbing, use ice. Cold constricts blood vessels, reducing inflammation and numbing the sharp pain. Apply an ice pack wrapped in a thin cloth for 15 minutes.
Moist Heat: If the pain feels like a stiff, tight “ache” (common with stress or poor sleep), heat is your friend. It increases blood flow and relaxes tight fibers. A hot shower is excellent, but a moist heating pad is even better. Avoid dry heat if possible, as it can sometimes dehydrate the superficial tissue.
3. The “Pain-Free Range” Rule

For the first 12 hours, you are on a “movement diet.” Avoid any movement that causes sharp pain. If turning your head to the left hurts, don’t do it repeatedly to “test” if it still hurts. Every time you provoke that sharp pain, you reset the inflammatory cycle. Keep your neck within a pain-free range of motion to let the tissues settle.
Step 2: The "Release" Phase (Hours 12–36)

Goal: Restore mobility through gentle, non-aggressive movement.
Once the acute guarding has settled (usually after a night of rest and the “Reset” protocols), you need to restore mobility. We do not use aggressive stretching here; we use neuromuscular input. We want to coax the muscles into lengthening, not force them.
1. The Chin Tuck (Cervical Retraction)

This is the gold standard exercise in physical therapy for neck pain. It reverses the “forward head posture” that dominates our modern lives (computer work, driving, scrolling).
How to do it: Sit upright with your chest lifted. Look straight ahead. Gently draw your chin straight back like you are making a “double chin” or sliding your head back on a shelf. Do not tilt your head up or down.
The Sensation: You should feel a gentle lengthening at the base of your skull and a release in the suboccipital muscles.
Prescription: Perform 10 repetitions, holding the “tucked” position for 3 seconds. Do this every 2 hours throughout the day.
2. Scapular Retraction (Shoulder Blade Squeezes)

The neck and the shoulder blades are intimately connected. Muscles like the Levator Scapulae and Trapezius attach from the neck directly to the shoulder blade. If your shoulders are rounded forward, these muscles are under constant tension.
How to do it: Sit or stand tall. Squeeze your shoulder blades together and down, as if you are trying to tuck them into your back pockets. Open your chest.
Prescription: Hold for 5 seconds, repeat 15 times. This creates a stable base for your neck to rest on.
3. Rotational Mobilization with Overpressure

Only attempt this if your pain level has dropped below a 5/10.
How to do it: Turn your head slowly to the stiff side just until you feel resistance (the “barrier”). Stop there. Place your hand on your cheek and apply very gentle pressure to guide your head 1-2 degrees further into the turn. Do not force through pain.
Breathing: Exhale as you turn. Inhale as you return to center.
Prescription: 5 gentle repetitions to each side.
Step 3: The "Re-engage" Phase (Hours 36–48)

Goal: Activate stabilizing muscles to prevent the pain from returning.
By day two, the sharp pain should be dulling into a general stiffness. Now you must re-engage the deep stabilizing muscles (the “core” of your neck) to support the spine. If you skip this step, the pain will likely return the moment you go back to your normal routine.
1. Isometric Strengthening

Isometrics involve muscle contraction without joint movement. This builds strength without grinding irritated joints, making it the perfect bridge between injury and full activity.
Front (Flexion): Place your hand on your forehead. Push your head forward into your hand, but use your hand to resist the movement so your head doesn’t move. Push at about 30% intensity. Hold 5 seconds.
Side (Lateral Flexion): Place your hand on the side of your head (above your ear). Push your head into your hand. Resist. Hold 5 seconds.
Back (Extension): Clasp hands behind your head. Push the back of your head into your hands. Resist. Hold 5 seconds.
Prescription: Perform 5 reps in each direction, 2-3 times a day.
2. The Ergonomic Audit

You cannot heal a neck that you reinjure 8 hours a day. During this phase, you must fix the environment that caused the problem.
Monitor Height: Your eyes should hit the top third of your screen. If you are looking down, you are increasing the load on your neck by up to 400%.
The Phone Rule: Bring your phone up to your eyes; do not drop your chin to your chest. “Text neck” is a real diagnosis, and it reverses all the progress you make with exercises.
Seat Position: Ensure your lower back is supported. If your lumbar spine slumps, your head automatically juts forward to compensate.
Signs You Need a Neck Pain Physical Therapist Appointment

While this 4-step method effectively resolves many cases of mechanical neck pain, it is not a cure-all. There are specific symptoms that indicate a more serious underlying issue that requires professional intervention.
You should book a neck pain physical therapist appointment immediately if you experience:
1. Cervical Radiculopathy
If you feel numbness, tingling, “pins and needles,” or weakness traveling down your arm or into your fingers, this suggests a nerve root is being compressed. This is not a muscle problem; it is a nerve problem. Ignoring this can lead to permanent muscle weakness.
2. Unrelenting or Night Pain
Mechanical pain usually gets better with rest. If your pain is constant, does not change with position, keeps you awake at night, or is accompanied by fever or unexplained weight loss, this is a major red flag requiring medical evaluation.
3. Trauma or Whiplash
If your neck pain is the result of a fall, car accident, or sports impact, do not attempt self-treatment. You need to rule out fractures or ligamentous instability before moving your neck.
4. Dizziness or Visual Disturbances
If moving your head causes dizziness, double vision, nausea, or nystagmus (rapid eye movement), this could indicate an issue with the vertebral artery or the vestibular system. This requires immediate professional assessment.
What to Expect During a Neck Pain Physical Therapist Appointment

If you decide to seek professional help, understanding the process can alleviate anxiety. A physiotherapy session is far more than just a massage. It is a diagnostic and therapeutic intervention.
The Evaluation
Your therapist will perform a comprehensive evaluation that includes:
Range of Motion Assessment: Measuring exactly how many degrees you can move in each direction.
Neurological Screening: Testing your reflexes, sensation, and muscle strength (myotomes) to ensure your nerves are healthy.
Palpation: Identifying exactly which spinal segment or muscle is causing the pain.
Joint Mobility Testing: Checking for hypomobility (stiffness) or hypermobility (instability) in the vertebrae.
Advanced Treatments
A neck pain physical therapist appointment gives you access to treatments you cannot do at home:
Manual Therapy: Skilled mobilization of the facet joints to “unlock” stiff segments.
Cervical Traction: Mechanical decompression to relieve pressure on discs and nerves.
Dry Needling: A technique using thin monofilament needles to release deep trigger points that fingers cannot reach.
Soft Tissue Mobilization: Specialized massage techniques (like Graston or ART) to break down scar tissue.
Long-Term Prevention: Living Pain-Free

Once you have successfully navigated the 48-hour window and reduced your pain, the goal shifts to prevention. You don’t want to be in this position again next month.
1. Pillow Talk: The Foundation of Sleep

We spend one-third of our lives sleeping. If your pillow is wrong, you are injuring yourself for 8 hours a night.
Side Sleepers: You need a thicker, firmer pillow to fill the “shoulder gap.” Your neck should remain horizontal, not tilted up or down.
Back Sleepers: You need a thinner pillow that supports the natural C-curve of the neck. Avoid propping your head up so high that your chin touches your chest.
Stomach Sleepers: This is the most traumatic position for the cervical spine because you must twist your head 90 degrees to breathe. Try to transition to side sleeping using a body pillow for support.
2. Hydration and Disc Health
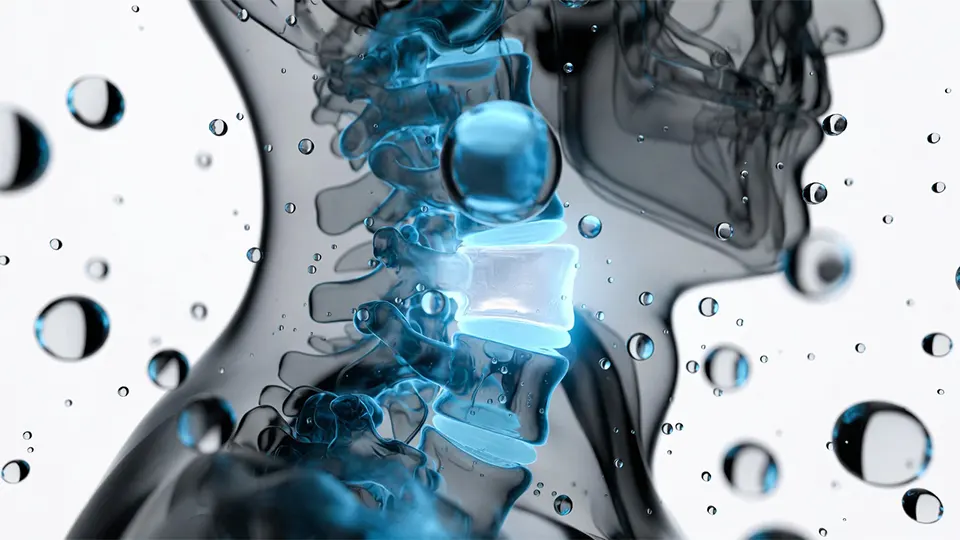
The discs between your vertebrae are avascular (poor blood supply) and rely on diffusion to get nutrients. They are also comprised largely of water. Dehydration can lead to disc desiccation (drying out), making them brittle and less able to absorb shock. Drinking adequate water throughout the day is a simple, biological way to protect your spine.
3. Stress Management

The upper trapezius muscles are often called the “stress muscles.” When we are anxious, we subconsciously shrug our shoulders toward our ears. This chronic tension compresses the cervical joints. Mindfulness techniques, diaphragmatic breathing, and regular exercise can lower your baseline muscle tension.
Conclusion
Neck pain does not have to be a life sentence of stiffness and headaches. By following this 3-Step Method (Reset, Release, Re-engage), you can often take control of acute symptoms within 48 hours. The key is to listen to your body—rest when needed, move gently when able, and strengthen to protect.
However, remember that pain is your body’s request for change. If your symptoms persist beyond a few days, or if the pain is recurrent, do not delay. Scheduling a neck pain physical therapist appointment is the fastest route to a full recovery. A physical therapist can provide the hands-on care, accurate diagnosis, and customized roadmap you need to get back to living pain-free.
Don’t wait for the pain to become chronic. Take action today, reset your spine, and move better tomorrow.
Frequently Asked Questions (FAQ)
How do I know if I need a neck pain physical therapist appointment or if I can just treat it at home?
If your pain is manageable (under 5/10), stays in the neck (doesn’t shoot down the arm), and improves with rest/heat within 2-3 days, home treatment is usually sufficient. If the pain is severe, involves arm numbness/weakness, or persists for more than a week, you should book an appointment.
Can a chiropractor help, or should I see a physical therapist?
Both can be helpful, but their approaches differ. Chiropractors often focus on spinal adjustments (manipulation) to restore alignment. Physical therapists focus on the entire system—mobilizing joints, releasing soft tissue, and significantly, prescribing exercises to strengthen muscles so the pain doesn’t come back. For long-term relief and prevention, physical therapy is often the preferred choice.
Is it safe to "crack" my own neck?
It is generally not recommended. When you crack your own neck, you are usually “cracking” the hypermobile (loose) segments above or below the stiff spot, rather than the stiff spot itself. This can lead to instability over time. A physical therapist performs targeted mobilizations only on the segments that need it.
How soon can I expect results from physical therapy?
Most patients feel relief after their very first session due to manual therapy techniques and traction. However, significant, lasting improvement typically takes 4 to 6 weeks of consistent care as the muscles strengthen and tissues heal.
What is "Text Neck"?
Text Neck is a repetitive stress injury caused by holding your head in a forward, downward position for extended periods while looking at a smartphone. This posture reverses the natural curve of the neck and places massive strain on the posterior neck muscles.
Can dehydration cause neck pain?
Indirectly, yes. Dehydration can lead to muscle cramping and spasms. Furthermore, spinal discs require hydration to maintain their height and cushioning ability. Staying hydrated is a simple way to support spinal health.









