Table of Contents
Let’s be real for a second—navigating health insurance can feel like trying to solve a Rubik’s cube blindfolded. You pay your premiums, you read the fine print (well, some of it), and yet, when you actually get hurt, you’re left wondering, “Is this actually going to be paid for?”

If you’ve ever dealt with chronic pain, a sports injury, or post-surgery rehab, you know that physiotherapy isn’t just a luxury; it’s a necessity. It’s the difference between limping for months and getting back to your morning run in weeks. But here is the kicker: not all plans are created equal, and many people leave money on the table simply because they don’t know which physiotherapy treatments covered by insurance they are entitled to.
Today, we are going to break down the essential treatments that really should be in your plan, why they matter, and how to advocate for your health. Grab a coffee (or a foam roller), and let’s dive in.
The Hidden Value of Physiotherapy

Before we get to the list, let’s talk about why this matters. Physiotherapy is often viewed by insurers as “rehabilitative”—meaning they only want to pay when you are already broken. But modern physio is also preventative.
When your insurance covers a broad range of treatments, everyone wins. You get better faster, and the insurance company actually saves money in the long run by avoiding expensive surgeries or chronic medication costs. It’s a no-brainer, right? Yet, we often have to fight for it.
Knowing exactly what physiotherapy treatments covered by insurance are standard—or should be standard—gives you the power to choose better plans during open enrollment or appeal a denied claim.
Top 10 physiotherapy treatments covered by insurance
1. Manual Therapy

What It Is
Manual therapy is the bread and butter of physiotherapy. This isn’t just a massage; it’s skilled hand movements intended to improve tissue extensibility, increase range of motion, and induce relaxation. We are talking about joint mobilization and manipulation.
Why It Should Be Covered
If your insurance claims to cover physio but excludes manual therapy, they are basically selling you a car without wheels. It is often the first step in reducing pain enough to actually perform exercises. It’s hands-on, effective, and fundamental to recovery.
2. Therapeutic Exercise Programs

What It Is
Therapeutic exercise are the “homework” part of physio. It involves specific movements designed to correct impairments and restore muscular and skeletal function. It’s not just “lifting weights”; it’s targeted strengthening, endurance training, and flexibility exercises monitored by a pro.
Why It Should Be Covered
You can’t just “crack” a back and expect it to stay fixed. Muscles need to be retrained to hold the alignment. Insurance plans that cover the manual work but not the supervised exercise time are missing the other half of the equation. This is where long-term healing happens.
3. Electrotherapy (TENS/NMES)

What It Is
Transcutaneous Electrical Nerve Stimulation (TENS) and Neuromuscular Electrical Stimulation (NMES) sound like sci-fi terms, but they are game-changers for pain management. These little machines use electrical currents to stimulate nerves and muscles.
Why It Should Be Covered
For many patients, TENS is a non-opioid alternative for chronic pain management. In a world where we are desperately trying to reduce reliance on painkillers, physiotherapy treatments covered by insurance must include these drug-free pain relief options.
4. Ultrasound Therapy

What It Is
No, this isn’t for seeing a baby. Therapeutic ultrasound uses sound waves to generate heat deep inside muscle tissues. This increases blood flow, relaxes muscle spasms, and speeds up the healing process.
Why It Should Be Covered
It is incredibly effective for soft tissue injuries like tendonitis or non-acute joint swelling. It’s a passive treatment that prepares the body for active recovery. Denying coverage for this is denying a faster route to inflammation reduction.
5. Acupuncture and Dry Needling

What It Is
While acupuncture is rooted in Traditional Chinese Medicine, dry needling is a modern Western approach focusing on trigger points in muscles. Both involve inserting thin needles into the skin to relieve pain and release tension.
Why It Should Be Covered
This is often a battleground with insurance companies. They like to label it “experimental” or “alternative,” but the clinical evidence for dry needling in treating myofascial pain is robust. If it gets a patient off painkillers and back to work, it deserves to be covered.
6. Hydrotherapy (Aquatic Therapy)

What It Is
Physiotherapy performed in water. The buoyancy reduces the weight bearing on joints, while the water resistance helps strengthen muscles.
Why It Should Be Covered
For elderly patients or those with severe arthritis, gravity is the enemy. Land-based exercises might be too painful. Hydrotherapy offers a unique environment where rehabilitation is possible when it otherwise wouldn’t be. It’s essential for specific demographics and should be a standard inclusion.
7. Vestibular Rehabilitation

What It Is
Ever stood up too fast and felt the room spin? Now imagine that feeling never stops. Vestibular rehab treats dizziness and balance disorders (like Vertigo) originating in the inner ear.
Why It Should Be Covered
Falls are a leading cause of injury, especially in older adults. Vestibular rehab prevents falls. It is literally a life-saving preventative measure. When we talk about physiotherapy treatments covered by insurance, omitting this is a massive oversight in patient safety.
8. Pelvic Floor Physiotherapy

What It Is
This focuses on the muscles, ligaments, and connective tissues in the pelvic region. It is vital for post-partum recovery, incontinence issues, and pelvic pain.
Why It Should Be Covered
For too long, this has been considered a “niche” or “optional” treatment. It’s not. It impacts quality of life daily. Coverage for pelvic health is a major gap in many standard insurance policies, and it’s high time that changed.
9. Shockwave Therapy

What It Is
Extracorporeal Shockwave Therapy (ESWT) uses acoustic waves to target chronic conditions like plantar fasciitis or tennis elbow that haven’t responded to other treatments.
Why It Should Be Covered
It sounds intense, but it’s non-invasive and often the last stop before surgery. If an insurance company refuses to pay for a few sessions of shockwave therapy but agrees to pay for a $20,000 surgery later, the math just doesn’t add up.
10. Ergonomic Assessments

What It Is
This involves a physiotherapist analyzing your workstation or home environment to prevent injury. It’s about fitting the job to the person, not the person to the job.
Why It Should Be Covered
We spend huge chunks of our lives sitting. Repetitive strain injuries are rampant. An ounce of prevention is worth a pound of cure here. Covering a one-time assessment can prevent years of chronic back and neck treatment claims.
What are the best ways to compare insurance plans for physiotherapy coverage?
Comparing insurance plans for physiotherapy can be tricky because coverage is often hidden in the fine print or bundled with other services.
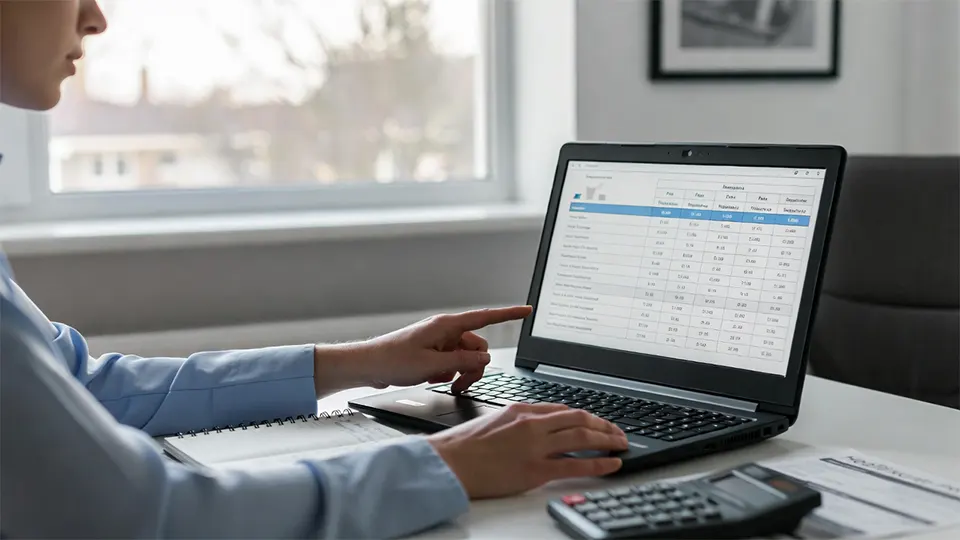
Here is a step-by-step guide and a comparison checklist to help you evaluate which plan offers the best value for physical therapy (PT).
1. The “Big Three” Cost Factors
When looking at a plan summary, look specifically for these three lines regarding “Outpatient Rehabilitation” or “Physical Therapy”:
| Feature | What to Look For | Why It Matters |
|---|---|---|
| Copay vs. Co-insurance | Copay: A flat fee (e.g., $30/visit).Co-insurance: A percentage (e.g., you pay 20%). | Copays are usually better for PT. If you have a 20% co-insurance and the therapist bills $300/session, you pay $60. A flat $30 copay saves you money. |
| Deductible | Does PT kick in before or after the deductible? | If you have a $2,000 deductible and PT is subject to it, you will pay the full cost of every session until you spend $2,000. Look for plans where PT is not subject to the deductible. |
| Visit Limits | Is there a “Hard Cap”? | Many plans limit you to 20 or 30 visits per year. Be careful—this often combines PT, Occupational Therapy, and Speech Therapy into one “bucket.” |
2. Check for “Medical Necessity” vs. “Open Access”
Some plans are strict gatekeepers, while others are more flexible.
Gatekeeper Plans (HMOs): You must see a primary care doctor first to get a referral. If you wake up with back pain, you can’t just go to the physio; you have to pay for a doctor’s visit first.
Direct Access Plans (PPOs): You can go straight to a physical therapist without a referral. This saves you time and the cost of the initial doctor’s copay.
3. The Hidden “Bundling” Trap
This is the most common trap. Insurers often bundle Physical Therapy with Chiropractic and Occupational Therapy.
The Trap: The plan says “60 visits per year,” which sounds great. But the fine print says “Combined limit for PT, Chiro, and OT.”
The Fix: Look for a plan that has a separate limit for Physical Therapy, or a combined limit that is high enough (e.g., 60+) to cover extensive rehab if you need surgery.
4. Comparison Checklist: Questions to Ask
When you are on the phone with an agent or comparing plan PDFs, use this checklist:
Is there a separate deductible for PT? (Ideally: No)
Is the visit limit “per condition” or “per year”? (Per condition is better; if you hurt your knee in March and your shoulder in August, you get a fresh set of visits.)
Do I need a referral or pre-authorization? (Referrals add administrative hassle and delay care.)
Are “modalities” covered? (Some cheap plans cover the exercise but deny claims for manual therapy, dry needling, or ultrasound.)
What is the Out-of-Network coverage? (Crucial if your preferred specialist isn’t in their network. varied coverage usually pays 50-70% of the “allowed amount,” not the billed amount.)
5. Red Flags 🚩
Avoid plans that use these terms regarding physiotherapy:
“Medical Necessity Review after 5 visits”: This means after just 5 sessions, they can cut you off if they think you aren’t improving “fast enough.”
“Improvement Standard”: Some plans deny coverage if you are maintaining function (preventing decline) rather than strictly improving. This is bad for chronic conditions.
“Therapy Cap”: A hard dollar limit (e.g., “We pay $1,500 max per year”). One bad injury can blow through this in a month.
How to Check Your Coverage

Now that you know what should be covered, how do you find out what is covered?
Call the Number on the Back of Your Card: Don’t rely on the booklet you got three years ago. Policies change.
Ask for CPT Codes: When your physio recommends a treatment, ask for the specific billing code (CPT code). Give this code to your insurance rep to get a definitive “yes” or “no.”
Appeal Denials: If a treatment that is medically necessary is denied, fight it. Have your physiotherapist write a letter of medical necessity.
Conclusion
Health insurance is a tool, and like any tool, it works best when you know how to use it. By understanding the wide array of therapies available, you can better advocate for your own care.
Ideally, physiotherapy treatments covered by insurance should encompass the full spectrum of recovery—from the initial pain relief of manual therapy to the long-term strengthening of therapeutic exercise. If your current plan falls short, it might be time to shop around during your next enrollment period.
Your body is the only place you have to live—make sure your insurance helps you take care of it!
Frequently Asked Questions (FAQs) About Physiotherapy Insurance
Do I need a doctor’s referral to see a physiotherapist?
It depends on your plan and where you live.
Many states and countries now have “Direct Access” laws, which means you can walk straight into a physiotherapy clinic without seeing a doctor first. However, some insurance plans (especially HMOs) still require a referral from your primary care physician to pay for the visit. Always call the number on the back of your card to double-check before booking.
My insurance says I have "30 visits per year." Does that mean 30 physiotherapy sessions?
Not necessarily.
This is a common “gotcha.” Often, that 30-visit limit is a combined cap for Physical Therapy, Occupational Therapy, and sometimes even Speech Therapy or Chiropractic care. If you are seeing a chiropractor and a physio, you might be drawing from the same pool of visits. Be sure to ask if the limit is “shared” or “dedicated.”
Why won't my insurance cover Dry Needling or Shockwave Therapy?
They often label it “Investigational” or “Experimental.”
Even though these treatments are widely used and supported by clinical evidence, insurance companies can be slow to update their policies. They may cover the physiotherapy visit itself (the evaluation and exercise part) but deny the specific billing code for dry needling, leaving you to pay a small “surcharge” or out-of-pocket fee for that specific service.
What happens if I use up all my covered visits but still need treatment?
You have a few options.
First, your physiotherapist can submit a request for “additional authorization” based on medical necessity. If that is denied, most clinics offer a discounted “cash-pay” or “self-pay” rate for patients who have exhausted their insurance benefits. It’s often cheaper than the billed insurance rate!
Does insurance cover "maintenance" physiotherapy?
Usually, no.
Insurance typically pays for rehabilitation (getting you back to your previous level of function) but not maintenance (keeping you there). Once you have reached a “plateau” where you aren’t significantly improving, insurance will often stop paying, even if the therapy stops you from getting worse. This is why learning your home exercise program is so critical!
What is the difference between a Copay and Co-insurance for Physio?
A Copay is a flat fee; Co-insurance is a percentage.
Copay: You pay $30, and insurance handles the rest. This is predictable and usually cheaper.
Co-insurance: You pay a percentage (e.g., 20%) of the total bill. Since initial evaluations can cost $200+, a 20% co-insurance could mean you pay $40+ per session.
Can I go to an "Out-of-Network" physiotherapist?
Yes, but it will cost you.
If you have a PPO plan, you can see an out-of-network provider, but you will likely have a higher deductible and higher co-insurance (e.g., paying 40-50% of the cost instead of 20%). However, some specialized clinics are worth the extra cost if they offer specific treatments (like advanced pelvic floor therapy) that in-network providers don’t.