Table of Contents
Special tests in physiotherapy are far more than routine checklists—they are precision tools that help clinicians uncover the root cause of a patient’s pain or dysfunction. By combining skilled observation, palpation, and targeted maneuvers, these tests provide invaluable insights into:
Joint integrity – detecting laxity, instability, or ligament damage
Muscle performance – assessing strength, endurance, and recruitment patterns
Neurological function – identifying nerve involvement or motor control deficits
Functional capacity – evaluating real-world movement patterns and balance

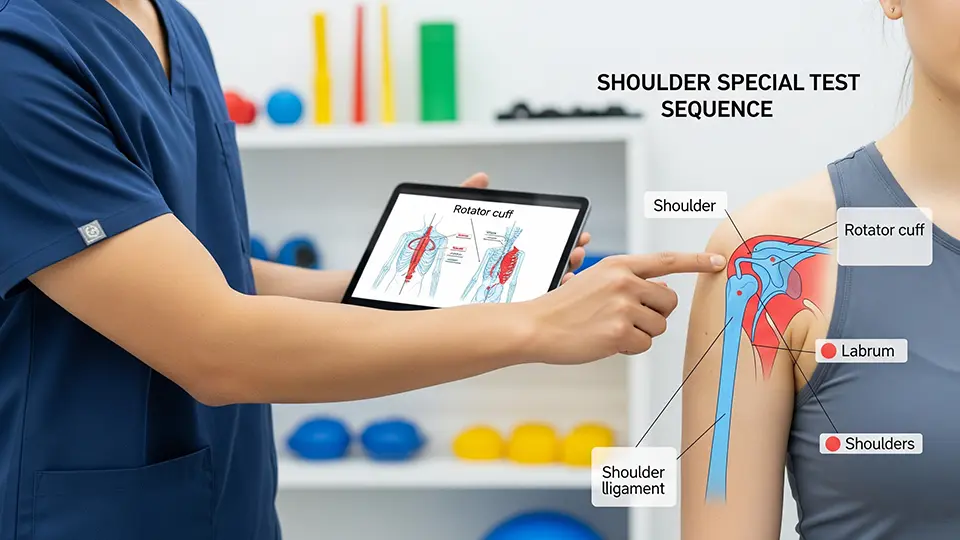
When it comes to the shoulder, special tests can differentiate between rotator cuff tears, impingement syndromes, labral lesions, biceps tendinopathy, and glenohumeral instability conditions that often share overlapping symptoms but require very different treatment approaches.
Similarly, in the realm of fall prevention and rehabilitation, standardized tools like the Berg Balance Scale (BBS) remain gold standards for objectively measuring a person’s static and dynamic stability. From elderly individuals at risk of falls to post-stroke patients relearning mobility, these tests provide measurable data that guide safe, effective rehabilitation plans.
This comprehensive guide is designed to be both educational and practical. Inside, you’ll find:
A complete list of shoulder special tests, each with its purpose, step-by-step instructions, and clinical interpretation tips.
A detailed overview of the Berg Balance Scale, including its 14 functional tasks and scoring system.
A downloadable quick-reference PDF, perfect for use in busy clinics, student study sessions, or home practice.
Whether you are a physiotherapist, sports rehab specialist, orthopaedic clinician, or physiotherapy student, this resource will equip you with evidence-based testing methods to improve diagnosis accuracy, enhance patient outcomes, and streamline your clinical workflow.
What Are Special Tests in Physiotherapy?
Special tests in physiotherapy are focused, evidence-based clinical procedures designed to assess the integrity, function, and stability of specific joints, muscles, ligaments, tendons, and neural structures. Unlike general movement screens which provide a broad overview of mobility and strength—special tests apply targeted mechanical stress, isolated muscle activation, or controlled positioning to reproduce symptoms, identify dysfunction, or confirm a suspected diagnosis.
These tests are a crucial part of orthopaedic assessment, as they allow physiotherapists to move from a general hypothesis to a specific, clinically supported conclusion. For example, while shoulder pain can stem from many causes, a sequence of shoulder impingement tests and rotator cuff special tests can help narrow down the exact structure at fault.
Main Categories of Special Tests
Orthopaedic Special Tests
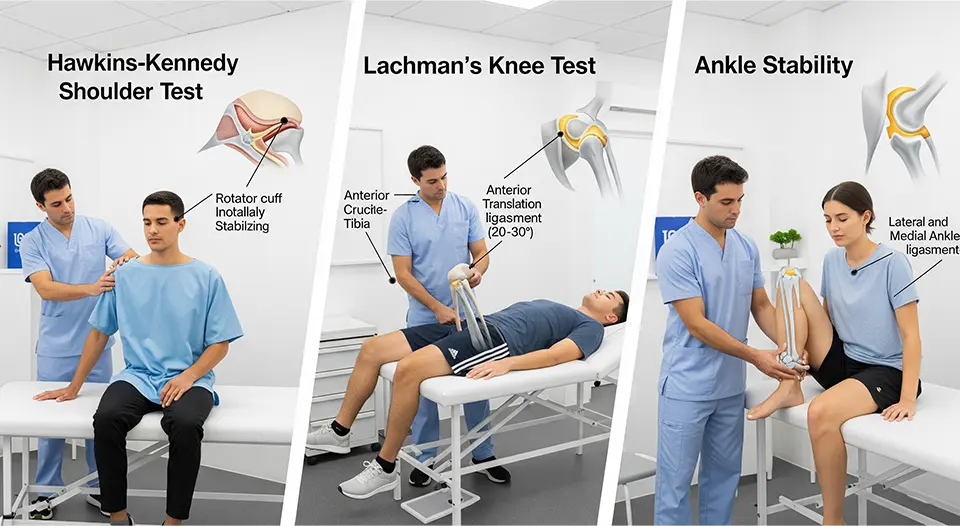
Used to evaluate musculoskeletal injuries and joint-related conditions.Shoulder: Neer Impingement Test, Hawkins-Kennedy Test, Apprehension Test, Drop Arm Test
Knee: Lachman Test, Anterior Drawer Test, McMurray’s Test
Hip: FABER Test, FADIR Test, Thomas Test
Neurological Special Tests
Designed to assess nerve health, tension, and conduction.Upper Limb Tension Tests (ULTTs)
Straight Leg Raise (SLR) Test
Deep tendon reflex assessments
Functional Balance & Mobility Tests
Measure dynamic and static stability, gait, and fall risk.Berg Balance Scale (BBS)
Timed Up and Go (TUG) Test
Functional Reach Test
Why Special Tests Matter in Physiotherapy
In modern physiotherapy practice, special tests are essential diagnostic and assessment tools that bridge the gap between a patient’s subjective symptoms and the objective clinical findings needed to create an effective treatment plan. They aren’t just about identifying the injured tissue—they influence the entire patient journey, from the first assessment to discharge.

1. Accurate Diagnosis & Differential Screening
Special tests allow clinicians to differentiate between multiple possible conditions that present with similar symptoms. For example, shoulder pain could stem from rotator cuff tendinopathy, labral tears, or impingement syndrome each requiring a different management approach. A well-chosen sequence of tests (e.g., Neer Impingement Test + Hawkins-Kennedy Test) can narrow the diagnosis quickly and accurately.
2. Determining Severity & Stage of Injury
Beyond identifying the structure involved, special tests help assess how severe the injury is whether it’s an acute partial tear, a chronic degenerative change, or a complete rupture. This distinction is crucial for setting safe rehabilitation timelines and managing patient expectations.
3. Guiding Evidence-Based Rehabilitation
By pinpointing the injured area and understanding the underlying mechanism, physiotherapists can design targeted, stage-appropriate treatment programs. For example:
Positive Apprehension Test → early stabilization and rotator cuff strengthening
Positive Drop Arm Test → progressive loading with careful avoidance of overhead stress in early rehab
4. Tracking Progress Over Time
Repeating specific tests during the course of treatment provides quantifiable benchmarks. Improvement in range of motion, strength, or pain response is a reliable indicator that the current rehab plan is working—or that adjustments are needed.
5. Enhancing Patient Education & Motivation
When patients see and feel the results of special tests—whether it’s the limitation on day one or the improvement weeks later—it builds trust, understanding, and engagement. It also makes abstract concepts (like “shoulder instability”) more tangible, improving compliance with home exercise programs.
6. Supporting Multidisciplinary Communication
Clear, test-based findings are valuable when collaborating with other healthcare professionals such as orthopedic surgeons, sports physicians, or occupational therapists. Test results provide a shared clinical language, ensuring consistent care across the team.
What Are Shoulder Special Tests?
Shoulder special tests are manual orthopedic assessment techniques performed by physiotherapists, orthopedic surgeons, sports medicine clinicians, and other rehabilitation professionals to evaluate the integrity, stability, and function of specific structures within the shoulder complex.

These tests go beyond a general examination—they are targeted maneuvers designed to provoke symptoms, assess joint mechanics, and identify potential injuries such as:
Rotator cuff tears (e.g., supraspinatus tear detected via the Empty Can test)
Labral lesions (including SLAP tears and Bankart lesions)
Shoulder impingement syndromes (subacromial, internal, or coracoid impingement)
Glenohumeral instability or recurrent dislocations
Biceps tendon pathology (tendinitis, tenosynovitis, or tendon rupture)
Acromioclavicular (AC) joint injuries
Scapular dyskinesis contributing to pain or movement restriction
Purpose and Clinical Relevance
The primary goal of shoulder special tests is differential diagnosishelping the clinician narrow down possible causes of shoulder pain or dysfunction.
When performed correctly, these tests provide:
Diagnostic clues to confirm or rule out suspected injuries
Objective data to support a working clinical hypothesis
Baseline measurements to track progress over time
How Shoulder Special Test Work
Most special tests involve placing the shoulder in a specific position and applying a controlled movement or resistance to stress certain tissues:
If the maneuver reproduces the patient’s familiar pain, it may indicate irritation or injury to that structure.
If weakness, apprehension, or abnormal movement occurs, it may suggest instability, tear, or neuromuscular impairment.
For example:
Hawkins-Kennedy Test → Compresses supraspinatus tendon against the coracoacromial arch to detect impingement.
Speed’s Test → Applies resistance to shoulder flexion to assess biceps tendon pathology.
O’Brien’s Test → Stresses the labrum to detect SLAP lesions.
The Golden Rule — Never in Isolation
While shoulder special tests are powerful, no single test is 100% accurate. A positive result alone doesn’t confirm a diagnosis—it must be interpreted alongside:
Patient history (onset, activity patterns, aggravating factors)
Observation and palpation (swelling, atrophy, tenderness)
Range of motion and strength testing
Imaging (MRI, ultrasound, X-ray) when appropriate
This multi-modal approach ensures accurate diagnosis, avoids false positives, and leads to better treatment outcomes.
Why Use Shoulder Special Tests?
Shoulder pain is one of the most frequent musculoskeletal complaints worldwide, with causes ranging from sports injuries and overuse syndromes to age-related degeneration and postural dysfunction. Whether the patient is an overhead athlete, a manual laborer, or an older adult struggling with daily tasks, one thing is clear: a precise, evidence-based assessment is essential to guide effective treatment.
Shoulder special tests—also called orthopedic shoulder examination tests—play a central role in this process. They are structured, reproducible maneuvers designed to stress specific anatomical structures, helping clinicians identify the root cause of pain or dysfunction.
1. Pinpoint the Source of Pain
By selectively loading tendons, ligaments, or joint capsules, special tests can help differentiate between:
Rotator cuff injuries (e.g., supraspinatus tear detected via the Empty Can or Drop Arm test)
Labral pathologies (e.g., SLAP tears assessed with O’Brien’s test)
Acromioclavicular joint problems (e.g., Cross-Body Adduction test)
Glenohumeral instability (e.g., Apprehension and Relocation tests)
This targeted approach reduces guesswork and avoids a “one-size-fits-all” treatment plan.
2. Reduce Unnecessary Imaging
While MRI and ultrasound can be valuable, they are costly, sometimes difficult to access, and not always needed in the early stages of assessment.
Using special tests early can help rule in or rule out common pathologies, guiding whether imaging is justified.
This approach saves time, reduces healthcare costs, and avoids over-reliance on scans that may detect incidental, non-symptomatic findings.
3. Select the Most Effective Treatment Plan
A precise diagnosis leads to targeted rehabilitation. For example:
Positive Hawkins-Kennedy test → Focus on subacromial decompression strategies.
Positive Speed’s test → Prioritize biceps tendon loading and stability work.
Positive apprehension → Emphasize stability and proprioception training before return to sport.
By aligning treatment with the specific injured structure, recovery is faster and outcomes are better.
4. Objectively Track Rehabilitation Progress
Special tests aren’t just for the first visit—they can be repeated to measure improvement:
Reduction in pain on provocative testing indicates healing and reduced inflammation.
Improvement in strength-based tests suggests restoration of functional capacity.
Patients can see and feel their progress, which boosts confidence and adherence to rehab.
5. Enhance Communication with Patients and Other Professionals
Clear special test results allow clinicians to:
Explain findings to patients in simple, visual terms (“This test tells us your rotator cuff is likely irritated”).
Share consistent data with surgeons, sports physicians, or insurance providers to justify ongoing treatment.
✅ Key Takeaway:
Shoulder special tests help bridge the gap between clinical reasoning and hands-on assessment. They allow physiotherapists, sports therapists, and orthopedic clinicians to deliver accurate, patient specific care while saving time, avoiding unnecessary imaging, and creating a clear roadmap for rehabilitation.
Shoulder Special Tests – Complete Reference Guide
These are the most widely used shoulder assessment tests in physiotherapy, orthopaedics, and sports rehabilitation. Each test is designed to identify specific pathologies, guide diagnosis, and inform rehabilitation planning.
1. Neer Impingement Test

Purpose: Detects shoulder impingement syndrome, particularly involving the supraspinatus tendon or long head of biceps.
How to Perform:
Patient sits or stands.
Examiner stabilizes the scapula with one hand.
With the other hand, passively flex the patient’s arm forward in internal rotation until it reaches full elevation.
Positive Sign: Pain in the anterior or lateral shoulder during the end range indicates subacromial impingement.
Clinical Tip: A positive Neer combined with a positive Hawkins-Kennedy test increases diagnostic confidence.
2. Hawkins-Kennedy Test

Purpose: Screens for subacromial impingement of rotator cuff tendons under the coracoacromial arch.
How to Perform:
Patient seated.
Examiner flexes the shoulder to 90° and elbow to 90°.
Internally rotate the humerus.
Positive Sign: Pain or discomfort suggests impingement, especially of the supraspinatus tendon.
Clinical Tip: Often performed after Neer’s Test for a more complete impingement assessment.
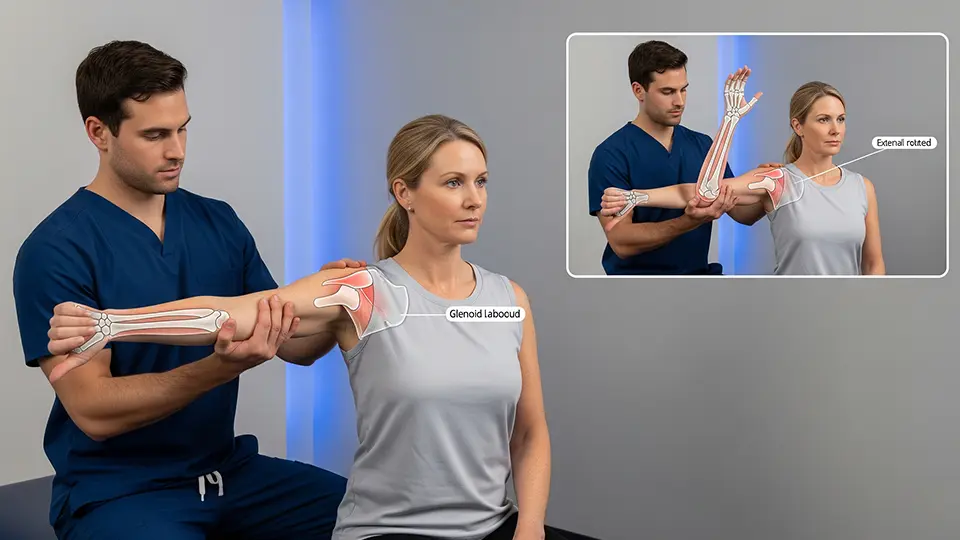
3. Apprehension Test (Anterior)
Purpose: Evaluates anterior shoulder instability due to capsulolabral injury or ligament laxity.
How to Perform:
Patient supine with shoulder abducted to 90° and elbow flexed to 90°.
Examiner slowly externally rotates the shoulder while applying gentle anterior pressure.
Positive Sign: Patient shows fear, apprehension, or resists further motion (rather than just pain).
Clinical Tip: Follow up with the Relocation Test to confirm instability vs. pain origin.
4. Speed’s Test

Purpose: Identifies biceps tendinopathy or superior labral lesions.
How to Perform:
Patient seated or standing with elbow extended and forearm supinated.
Examiner resists shoulder flexion at about 90°.
Positive Sign: Pain in the bicipital groove indicates pathology of the long head of biceps tendon.
Clinical Tip: Palpate the groove during the test to localize pain more accurately.
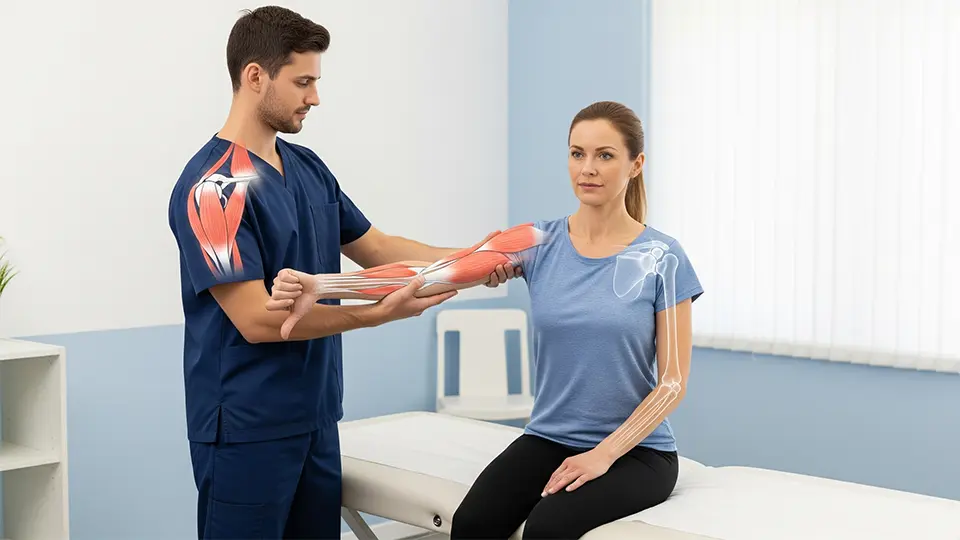
5. Empty Can Test (Jobe’s Test)
Purpose: Tests supraspinatus muscle and tendon integrity.
How to Perform:
Patient abducts arms to 90° in the scapular plane and internally rotates so thumbs point downward.
Examiner applies downward pressure while the patient resists.
Positive Sign: Weakness or pain indicates supraspinatus tear or tendinopathy.
Clinical Tip: Compare bilaterally to detect subtle strength deficits.
6. Lift-off Test

Purpose: Evaluates subscapularis muscle function.
How to Perform:
Patient places the back of their hand on the lower back.
Attempts to lift the hand away from the back against resistance.
Positive Sign: Inability to lift the hand off the back suggests subscapularis weakness or tear.
Clinical Tip: If patient can’t get into starting position due to limited mobility, try the Belly Press Test instead.
7. Sulcus Sign

Purpose: Indicates inferior glenohumeral instability or capsular laxity.
How to Perform:
Patient seated with arms relaxed.
Examiner pulls the arm downward at the elbow.
Positive Sign: Visible sulcus (gap) between the acromion and humeral head.
Clinical Tip: Grade the laxity (mild, moderate, severe) and compare both sides for baseline.
8. O’Brien’s Test (Active Compression Test)
Purpose: Detects SLAP lesions or AC joint pathology.
How to Perform:
Patient flexes shoulder to 90°, adducts 10–15°, and internally rotates (thumb down).
Examiner applies downward pressure while patient resists.
Repeat with palm up (external rotation).
Positive Sign: Pain with thumb down that reduces or disappears with palm up suggests labral lesion; pain over AC joint may indicate AC pathology.
Clinical Tip: Always interpret in context of other labral tests (Crank Test, Biceps Load Test).
💡 Pro Tip for Clinicians:
For maximum diagnostic accuracy, avoid relying on a single test. Combining two or more that target the same pathology (e.g., Neer + Hawkins for impingement, Apprehension + Relocation for instability) increases both sensitivity and specificity.
Deep Dive Example: Berg Balance Scale (BBS)
While shoulder special tests focus on diagnosing joint stability, muscle integrity, and tendon health, the Berg Balance Scale (BBS) is a gold standard assessment tool used to evaluate a person’s functional balance abilities through 14 structured tasks that mirror real-life movements.

Origin and Development
The Berg Balance Scale was created in the late 1980s by Dr. Katherine Berg, a Canadian physiotherapist and researcher.
Initially designed to identify fall risk in older adults.
Over time, its use expanded into neurological rehabilitation, orthopedic recovery, and research-based outcome measures.
Today, it’s one of the most frequently cited balance assessment tools in physiotherapy literature.
Purpose and Clinical Applications
The BBS is more than just a test—it’s a quantitative tool for measuring postural stability and guiding treatment plans. It helps clinicians:
Quantify static and dynamic balance performance
Detect early signs of instability before falls occur
Track rehabilitation progress objectively over time
Support discharge planning by measuring readiness for community mobility
Provide evidence-based data for insurance documentation and outcome tracking
Who Benefits From the Berg Balance Scale?

The BBS is used across multiple patient populations, including:
Older adults – to screen for fall risk and guide fall-prevention programs.
Stroke survivors – to assess balance deficits and monitor neuro-rehabilitation gains.
Parkinson’s disease patients – to measure functional balance decline and progression.
Multiple sclerosis patients – to identify balance impairments linked to central nervous system changes.
Post-orthopedic surgery patients – e.g., after hip fracture or knee replacement, to evaluate safe mobility.
Vestibular disorder patients – to track balance recovery after vestibular rehab.
The 14 Tasks of the Berg Balance Scale (BBS)

| Task # | Description | Max Score |
|---|---|---|
| 1 | Sitting to standing | 4 |
| 2 | Standing unsupported | 4 |
| 3 | Sitting unsupported | 4 |
| 4 | Standing to sitting | 4 |
| 5 | Transfers | 4 |
| 6 | Standing with eyes closed | 4 |
| 7 | Standing with feet together | 4 |
| 8 | Reaching forward with outstretched arm | 4 |
| 9 | Retrieving object from floor | 4 |
| 10 | Turning to look behind | 4 |
| 11 | Turning 360 degrees | 4 |
| 12 | Placing alternate foot on stool | 4 |
| 13 | Standing with one foot in front | 4 |
| 14 | Standing on one leg | 4 |
Total Possible Score: 56 points
Scoring and Interpretation
41–56 points: Low fall risk
21–40 points: Medium fall risk
0–20 points: High fall risk
Lower scores indicate poorer balance control and higher likelihood of falls.
Advantages of the Berg Balance Scale (BBS)
The Berg Balance Scale has earned its place as one of the most trusted functional balance assessments in clinical practice—not just because it’s widely recognized, but because it delivers practical, evidence-based benefits for both therapists and patients.

1. Quick to Administer (10–15 Minutes)
Time efficiency is critical in busy clinical environments. The BBS can be completed in under a quarter of an hour without sacrificing accuracy or reliability.
Ideal for initial evaluations when time is limited.
Perfect for follow-up sessions to track progress without taking up the whole appointment.
Allows therapists to integrate balance testing into broader assessments without overburdening the session.
2. No Special Equipment Required
Unlike some balance assessments that require force plates, motion capture systems, or expensive lab setups, the BBS only requires:
A standard chair with armrests.
A stopwatch or timer.
A small object (such as a pen) to pick up.
A step or stool (for one of the tasks).
This makes it cost-effective and accessible for:Private physiotherapy clinics.
Hospital outpatient departments.
Home visits and community-based rehabilitation.
3. Validated in Multiple Populations
The BBS isn’t limited to one type of patient—it has been extensively validated across demographics and medical conditions, including:
Older adults at risk of falls.
Neurological patients (stroke, Parkinson’s disease, multiple sclerosis).
Post-orthopedic surgery patients (hip fracture, knee replacement).
People with vestibular disorders.
This cross-population validity means therapists can confidently apply the test in diverse clinical scenarios without worrying about its relevance.
4. Predictive of Fall Risk
One of the most significant advantages of the BBS is its predictive power.
Low scores strongly correlate with increased likelihood of falls within the next 6–12 months.
Enables clinicians to intervene early with fall-prevention strategies.
Helps educate patients and caregivers about safety, mobility aids, and exercise programs tailored to risk level.
5. Easily Repeatable for Progress Monitoring
Because the BBS uses clear scoring criteria and requires minimal setup, it can be repeated frequently to:
Monitor rehabilitation progress objectively.
Adjust treatment plans based on quantitative improvements or plateaus.
Provide visual proof of progress to patients, boosting motivation and adherence.
6. Globally Recognized and Research-Supported
The BBS is cited in hundreds of peer-reviewed studies, ensuring clinicians can reference strong evidence when justifying its use to insurers, other healthcare professionals, or in academic work.
Its inclusion in international rehabilitation guidelines further reinforces its role as a gold standard tool in balance assessment.
Download PDF of Shoulder speical tests
Expanded_Berg_Balance_Scale_Guide
Conclusion
Special tests are vital in physiotherapy for accurate diagnosis and targeted rehab. For shoulder injuries, tools like the Neer and Hawkins-Kennedy tests offer diagnostic precision, while the Berg Balance Scale remains a gold standard for assessing and improving patient stability.
By combining orthopedic and functional assessments, physiotherapists can create more effective, individualized treatment plans — improving patient safety and long-term outcomes.
FAQs About Shoulder Special Tests
What are shoulder special tests used for?
They are targeted physical examination techniques that help identify injuries or dysfunctions in the shoulder, such as rotator cuff tears, impingement, labral injuries, instability, and AC joint problems.
Can I diagnose a shoulder injury with just one special test?
No — no single test is 100% accurate. Results must be interpreted with patient history, observation, palpation, ROM testing, and possibly imaging for a complete diagnosis.
Are shoulder special tests painful?
Some may cause temporary discomfort if they reproduce the patient’s symptoms, but they should not cause lasting pain if performed correctly.
How accurate are shoulder special tests?
Accuracy varies by test. For example, the Hawkins-Kennedy test has around 80% sensitivity for impingement, while O’Brien’s test has higher specificity for SLAP lesions. Using test clusters improves accuracy.
Who can perform shoulder special tests?
They are typically performed by physiotherapists, sports medicine doctors, orthopedic specialists, athletic trainers, and rehabilitation professionals trained in musculoskeletal assessment.
Can I perform shoulder special tests at home?
Some movements can be tried for self-assessment, but interpretation requires professional training. Self-diagnosis is not recommended — always consult a qualified clinician.
What are the most common shoulder special tests?
Some of the most used include:
Hawkins-Kennedy Test – Impingement
Neer’s Test – Impingement
Empty Can Test – Rotator cuff tear
O’Brien’s Test – SLAP lesion
Apprehension & Relocation Tests – Instability
Why are these tests important for physiotherapists?
They allow physiotherapists to pinpoint the exact source of dysfunction, develop tailored treatment plans, and track progress over time with objective, reproducible measures.
📢 Call-to-Action (CTA)
Ready to take your shoulder assessment skills to the next level?
💪 Download our FREE Printable Shoulder Special Tests Quick-Reference PDF — perfect for clinic use, student revision, or on-the-go assessments.
✅ Includes step-by-step instructions for 15+ essential tests
✅ Evidence-based accuracy notes & clinical pearls
✅ Organized for fast, real-world application
📥 Click Here to Download Your Shoulder Special Tests PDF Now
And don’t forget — bookmark this page for instant access to testing guides, rehab tips, and physiotherapy resources updated monthly!










2 thoughts on “Special Tests in Physiotherapy: Shoulder Special Test & the Berg Balance Scale – Complete Guide with Scores, Instructions & PDF”
Very interesting info !Perfect just what I was searching for! “The only limit to our realization of tomorrow will be our doubts about reality.” by Franklin Delano Roosevelt.
Solid arguments